Built For Orthopaedic Trauma
From articular to periprosthetic fractures, every step of our development is guided by real-world surgeon feedback, current clinical practice and scientific evidence.

Our Medical Advisors

Karl-Heinz
Frosch
Medical Director – UKE and BG Klinikum Hamburg

Anna N.
Miller
Jerome J. Gilden, MD, Chair & Professor –
Dartmouth Health

H. Claude
Sagi
Professor of Clinical
Joseph S. Stern Jr. Endowed Chair in Orthopaedic Surgery – University of Cincinnati Medical Center

Michael J.
Weaver
BWH Distinguished Chair in Orth. Surgery
Associate Professor Harvard Medical School

Rich
Yoon
Clinical Professor of Orthopaedic Surgery, Rutgers-RWJBH, New Brunswick, NJ
Selected Publications
Enabling Technology in Fracture Surgery: State of the Art
Three-dimensional (3D) printing and virtual modeling, using computed tomographic (CT) scans as a base for the 3D-printed model, help surgeons to visualize relevant anatomy, may provide a better understanding of fracture planes, may help to plan surgical approaches, and can possibly simulate surgical fixation options. Navigation systems create real-time 3D maps of patient anatomy intraoperatively, with most literature in orthopaedic trauma thus far demonstrating efficacy in percutaneous screw placement using preoperative imaging data or intraoperative markers. Augmented reality and virtual reality are new applications in orthopaedic trauma, with the former in particular demonstrating the potential utility in intraoperative visualization of implant placement. Use of 3D-printed metal implants has been studied in limited sample sizes thus far. However, early results have suggested that they may have good efficacy in improving intraoperative measures and postoperative outcomes.
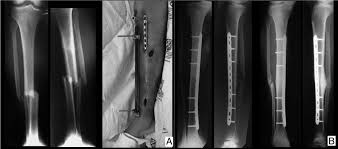
Is It Safe to Prep the External Fixator In Situ During Staged ORIF of Bicondylar Tibial Plateau Fractures? A Retrospective Comparative Cohort Study
To compare the risk of deep infection and unplanned reoperation after staged open reduction internal fixation (ORIF) of bicondylar tibial plateau (BTP) fractures whether elements of the temporizing external fixator were prepped into the surgical field or completely removed before definitive fixation.
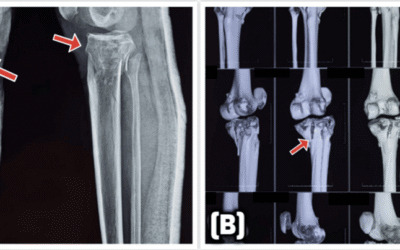
Fracture characteristics and functional outcomes for Schatzker V/VI bicondylar tibial plateau fractures with a separate tubercle fragment: a comparative study
A separate tibial tubercle fragment (TF) is found in up to half of all bicondylar tibial plateau (BTP) fractures. Adequate healing of the TF is required to reconstitute the extensor mechanism of the knee. The purpose of this study was to compare outcomes after surgical fixation of BTP fractures with and without a TF.
The repair capacity spectrum of human skeletal muscle injury from sports to surgical trauma settings
Skeletal muscle injury and repair have been a major research focus for more than a century. Muscle injuries are defined by their cause and anatomical location and lie on a spectrum in terms of repair outcomes. From contraction-induced necrosis, which initiates regenerative myogenesis for complete restoration of tissue architecture and function to, at the other end of the spectrum, traumatic volumetric muscle loss (VML), where substantial portions (or the whole) of a muscle are lost, leaving the patient with permanent physical disability. Strain injuries are found between these two extremes and are characterised by healing with scar tissue formation and a high re-rupture rate. Across these injury types, a discriminating feature for a successful outcome is the preservation of the extracellular matrix (ECM) architecture of the muscle-tendon complex, in particular the myotendinous junction (MTJ). Numerous experimental models, imaging techniques and molecular analyses have led to a thorough understanding of how muscle stem cells interact with immune, vessel and stroma-associated cells during regenerative myogenesis. Paradoxically, treatment of muscle strain injury and VML has not improved, and regenerative engineering approaches remain a distant hope. Important issues for this field include matching the level of detail that exists for animal muscle regeneration with human data and identifying the site of tissue disruption during strain injury. We propose that a closer collaboration between cell biologists, physiologists, sports medicine practitioners and orthopaedic surgeons is required to improve patient outcomes, particularly for strain injuries and VML.
Bicondylar tibial plateau fracture dislocations with an intact anterolateral cortical Rim: Prevalence, fracture characteristics, and complications
Bicondylar tibial plateau (BTP) fracture-dislocations with an intact anterolateral (AL) cortical rim present a unique treatment challenge due to posterolateral joint impaction. The purpose of this study was to determine the prevalence of this pattern within a large cohort of bicondylar tibial plateau fractures and describe fracture characteristics and complication rates.
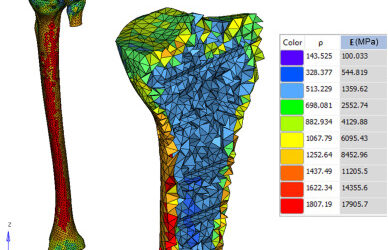
Segmentation and finite element analysis in orthopaedic trauma
Finite Element Analysis (FEA) has evolved into a crucial tool in orthopaedic trauma research and clinical practice. This review explores the broad applications of FEA in orthopedic surgery.
Weight bearing after surgical treatment of tibial plateau fractures – an international survey of orthopaedic trauma surgeons
The optimal postoperative weight-bearing regimen for tibial plateau fractures (TPF) remains a topic of debate. It ranges from non- or touch down- weight bearing between 2-12 weeks. More recent studies suggest that early weight-bearing may not result in any loss of reduction or hardware failure.
Open tibial plateau fractures: Infection rate and functional outcomes
Open tibial plateau fractures are complex injuries that require specialized management to prevent complications. The objective of this study was to compare the infection risk and functional outcomes between open and closed tibial plateau fractures.
Complications and timing of soft tissue coverage after complete articular, open tibial plateau fractures
Complete articular tibial plateau fractures are typically high-energy injuries associated with significant soft tissue trauma. The primary aim of this study was to evaluate the incidence of wound complications and need for soft tissue coverage after open, complete articular tibial plateau fractures.
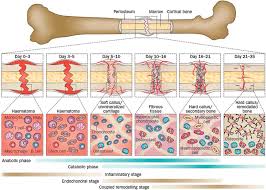
Influence of the fixation stability on the healing time–a numerical study of a patient-specific fracture healing process
The healing outcome of long bone fractures is strongly influenced by the interfragmentary movement of the bone fragments. This depends on the fixation stability, the optimum value of which is still not known. The aim of this study was to simulate a patient-specific human healing process using a numerical algorithm and to retrospectively analyse the influence of the fixation stability on the healing time.
Comparative analysis of tibial plateau fracture osteosynthesis: A finite element study
This study presents a comparative structural finite element analysis between two different fixation methods for high-energy tibial plateau fractures: limited contact dynamic compression plate (LC-DCP) and locking compression plate (LCP).
Physical and biological aspects of fracture healing with special reference to internal fixation
Fracture healing is a repair process of a mechanical discontinuity loss of force transmission, and pathological mobility of bone.
Failure of fixation of tibial plateau fractures
Forty-two consecutive patients treated surgically at our trauma unit for tibial plateau fractures were studied retrospectively, specifically for loss of fixation. Factors that might affect the fracture fixation were reviewed, including age, mechanism of injury, type of fracture, bone quality, severity of fragmentation, severity of displacement, time to surgery, operating time, fixation method, use of bone graft, postoperative bracing, and mobilization.
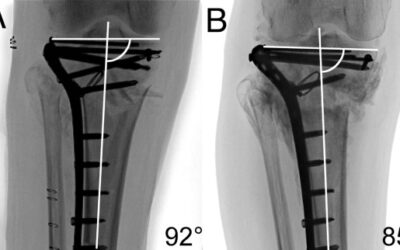
Fracture pattern and fixation type related to loss of reduction in bicondylar tibial plateau fractures
Bicondylar tibial plateau fractures can be treated with locked plating applied from the lateral side with or without additional application of a medial plate (dual plating). Recent studies demonstrate that these injuries can be sub-grouped based upon their morphology by computed tomography (CT).
Predictors of reduction loss in tibial plateau fracture surgery: Focusing on posterior coronal fractures
Some studies have reported that fracture pattern was associated with reduction loss after surgery. The purpose of this study was to evaluate various factors that can influence reduction loss, including fracture patterns in unicondylar and bicondylar tibial plateau fractures.
Radiographic Predictors of Conversion to Total Knee Arthroplasty After Tibial Plateau Fracture Surgery: Results in a Large Multicenter Cohort
Radiographic measurements of initial displacement of tibial plateau fractures and of postoperative reduction are used to determine treatment strategy and prognosis. We assessed the association between radiographic measurements and the risk of conversion to total knee arthroplasty (TKA) at the time of follow-up.

“Very valuable for trauma surgery”
– Karl-Heinz Frosch, Chair of Orthopedics, University Medical Center Hamburg-Eppendorf

“Quick and efficient”
– Rich Yoon, Clinical Chief of Orthopedics, RWJBarnabas Health

“A big step forward.”
– Anna Noel Miller, Chair of Orthopedics, Dartmouth Health